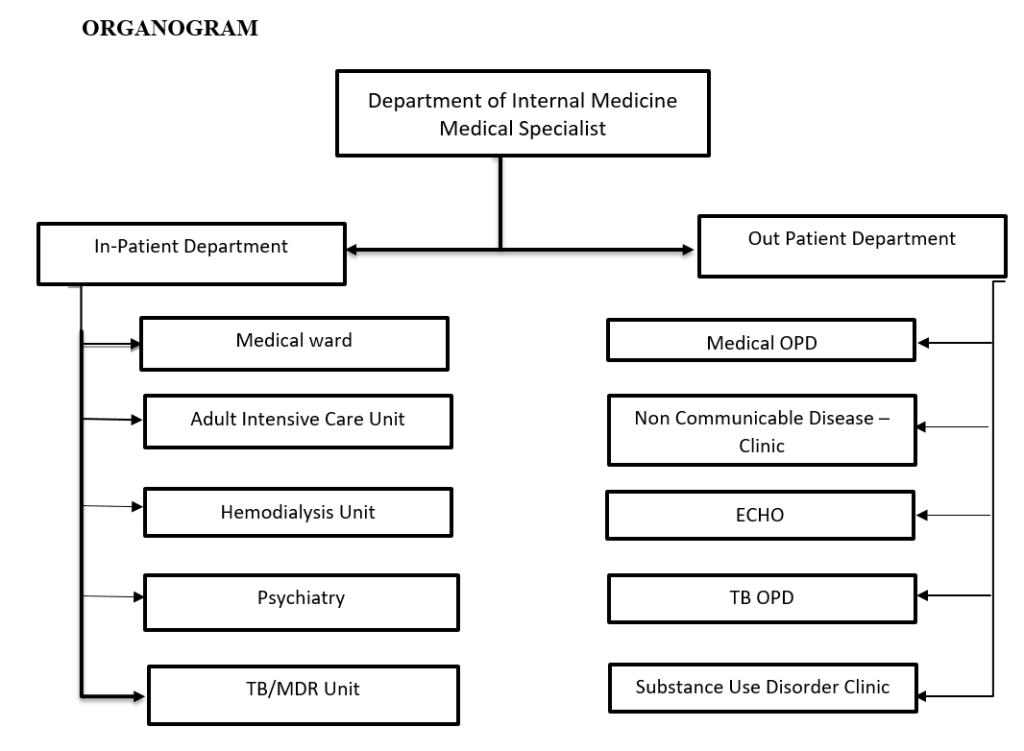
The Department of Internal Medicine provides inpatient and outpatient care which includes emergency, intensive and specialized care for patients requiring services like cardiology, nephrology/dialysis, gastroenterology, neurology, respiratory and non- communicable disease (NCD) clinics.
It also provides medical consultations to admitted patients in other departments. Additionally, the department also oversees the Substance Use Disorder (SUD) treatment and care services, individual, group and family therapy, and detoxification and referral to rehabilitation centers.
Since the establishment of Mongar hospital as Eastern Regional Referral Hospital in 1996 and upon completion of construction of the new hospital in 2007, the Department of Internal Medicine was shifted to second floor of the building (2008) which was then known as ‘Unit One’ and was functioning under one In-Charge ship in combination with the Department of Pediatrics. On 3rd June, 2017, Medical Extension Ward was established to accommodate an increasing number of medical patients and also to segregate TB patients for infection control.
In 2020, the Department of Internal Medicine was separated from the Department of Pediatrics. The then Medical Ward was merged with the Medical Extension Ward on the third floor and has been functioning as a full-fledged Medical Ward. It is headed by the Medical Specialist(s) and run by Nurse In-Charge, nurses and support staffs. In addition, the medical specialist oversees Adult Intensive Care Unit (AICU), Hemodialysis Unit (HDU), Psychiatric Unit, MDR-TB Unit and OPD services – Medical OPD, NCD clinic, Echo, SUD clinic, and TB clinic.
Vision
A health care unit providing an evidence-based holistic medical and nursing care services with an ambient teaching and learning environment.
Mission
- Provide an evidence-based medical treatment to acute and chronic medical conditions
- Provide evidence-based holistic nursing care to admitted patients
- Provide psychoeducation and counseling to patients with SUD and mental illnesses
- Provide DOTs to drug susceptible TB patients
- Foster an environment of teaching and learning
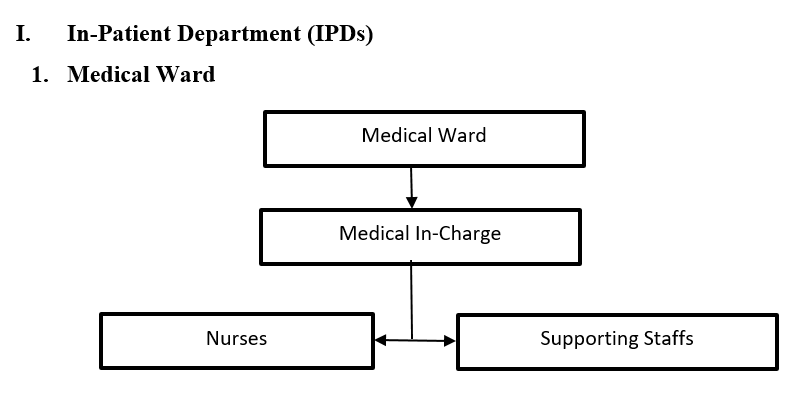
The Medical Ward has 33 beds of which 4 beds are designated for stroke patients, 12 beds for medical patients, 8 beds for psychiatric patients and 9 beds for TB patients.

1.1 Medical Cubicle
The second and third cubicles of the medical wing on the left side are dedicated for medical patients: a total of 12 beds – 6 in each cubicle. Medical patients are admitted here after triaging by the admitting nurse(s). Patients from medical OPD, Emergency, other wards (Transfer-In) and those referred from other Districts are admitted here.

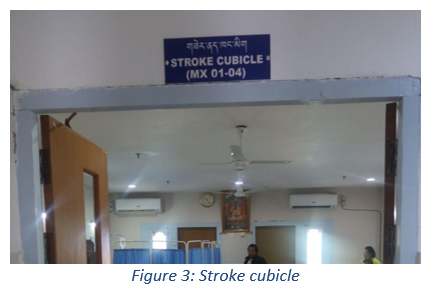
1.2 Stroke cubicle
ERRH is designated as one of the Stroke Centers in the country and is the only stroke care center for the 7 eastern districts. The “Stroke cubicle” was inaugurated in 2022 – first cubicle of the medical wing on the left side. There are 4 dedicated beds with side rails, monitors at head end, position changing charts, stroke care articles and the resuscitation trolley. This cubicle also functions as high dependency unit for acute/severe medical conditions along with resuscitation as it has all the amenities required.
1.3 Psychiatric cubicle
It has 8 beds allocated for the management of patients with psychiatric conditions of which 2 beds are designated for management of psychiatric emergency cases. In the absence of a psychiatrist, patients with mental illness, alcohol and substance use disorders are admitted and managed by medical specialist(s), counsellor and also emergency physician. The unit receives admissions directly from OPD, ER, and SUD clinics.
Common admissions seen are patients with alcohol use disorder (AUD) for detoxification and other mental health problems such as anxiety disorders and depression. Individual and group counseling are provided to patients and family members by the rounding specialist and a psychiatric nurse.
1.4 TB Cubicle
This cubicle has 9 beds allocated for the management of drug susceptible Tuberculosis (TB) patients. The patient is shifted to manage at MDR-TB ward which is located outside the hospital whenever there are MDR-TB patients. This is done mainly to reduce the risk of disease transmission in the ward and also to address human resource shortage. However, there are an adequate infection prevention and control (IPC) measures put in place when patient is admitted. This cubicle also functions as Isolation Room for contagious and transmissible diseases and as infection control unit for specific immuno-compromised patients to prevent them from getting infection from other patients.
Key Activities
Apart from the routine and individualized patient care, the unit also conducts following activities which are aimed for professional development of the staff, improving patient care services and enhancing patient safety;
- Fortnightly CME (Continuing Medical Education)
- Monthly 5-S CQI (Continuing Quality Improvement) activity
- Quarterly Unit Meeting
- Yearly POCQI (Point of Care Quality Improvement – 1 project minimum)
Services
The staff in medical ward also offer following services to in-patients and attendants;
- NCD screening (CVD Risk Assessment) for all patients and attendants above 40 years of age and those with risk factors
- Detoxification for alcohol and other substances
- Counseling services especially to alcoholic and SUD patients
- Monthly Health Education to patients and attendants
Way forward
- Sustain the current practice of Continuing Medical Education (CME)
- Sustain the yearly POCQI project to improve patient care
- Teaching, learning and conducting research
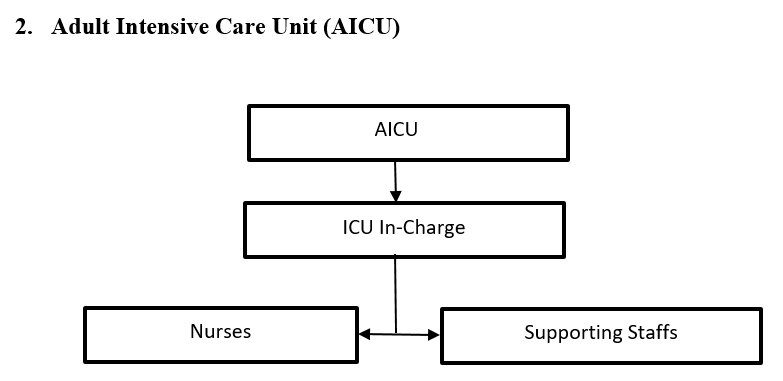
The Adult Intensive Care Unit (AICU) including Pediatric Intensive Care Unit (PICU) is a combined unit that came into service in June 2008. Initially there were five beds. With increasing admissions, bed capacity was increased to seven (5 for adults & 2 for pediatrics) in November 2022.
The patients in AICU are managed by the respective specialists. The unit takes care of all cases of critically ill patients. Patients are actively managed with a multidisciplinary approach involving the pharmacy, dieticians, physiotherapy professionals and other aspects of specialized care

Services provided
- 1. Main function of ICU is to provide optimum support adequate ICU care and monitoring of critically ill patients.
- 2. Invasive procedures are carried out at bedside especially like Central line insertion, Intercostal drainage, Endotracheal Intubation and ABG blood sampling.
- 3. Following are a list of nursing care standards (Care bundle) followed in the unit to prevent HCAI (Health Care Associated Infection).
a. VAP bundle
b. CAUTI bundle
c. CLABSI bundle
A “bundle” is a group of evidence-based care components for a given disease that, when executed together, may result in better outcomes than if implemented individually.

- 4. Other nursing care and activities in AICU/PICU
The ICU nurses also performs numerous other tasks like regular vital signs and mechanical ventilator findings, ventilator weaning assessment, monitoring sedation and pain level, formulation of Nursing Care Plan and documentations.
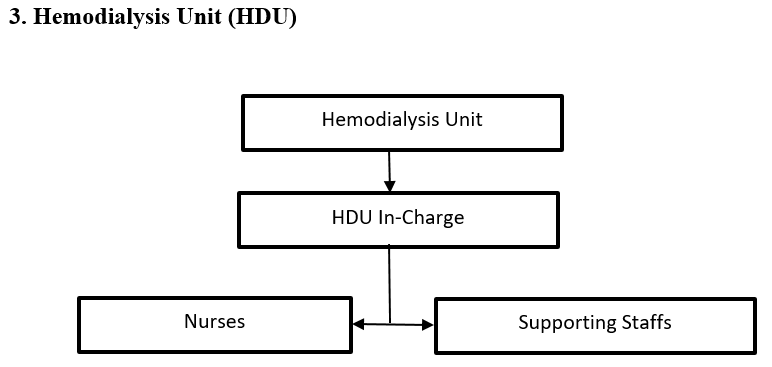
The Hemodialysis Unit was inaugurated on 12thSeptember, 2009 by the then Medical Superintendent Dr. Tapas Gurung and Lam Neten Ngawang of Mongar Dratshang. Initially it started with 2 dialysis machines which has subsequently increased to 4 t present. The HDU caters dialysis service for patients from 6 eastern districts and Bumthang.
Initially, there was 2 patients undergoing dialysis which has increased to 41 at present.

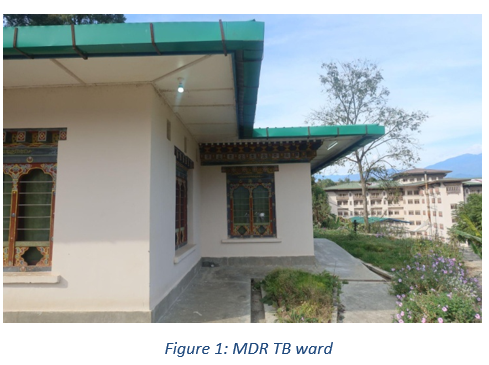
4. MDR-TB Ward
A new MDR-TB ward was inaugurated in April 2023. It is located near the hospital main water tank, away from the main hospital and has 6 beds. The ward is manned by nurses from different indoor units on rotation basis depending on the requirement. Medical Ward In-Charge oversees the day-to-day functioning of this ward. Apart from MDR-TB patients, drug susceptible patients too are managed here with all necessary precautions.
II. Out Patient Department (OPDs)
1. Substance Use Disorder (SUD) Clinic
Hospital-based Substance Use Disorder (SUD) Treatment and Care services was formally launched at The Pema Center, Thimphu, by Her Majesty the Gyaltsuen during commemoration of World Mental Health Day on 10th October, 2022. To launch the same service at ERRH, relevant staff were trained in January 2023 and formally service was launched on 21thFebruary 2023 coinciding with the 43rdbirth anniversary of His Majesty the King. The services of the then Drop-In-Center (DIC), BNCA of Mongar was brought under the SUD treatment services of ERRH to streamline and enhance the services. The Group Counselling Hall was furnished with all necessary with necessary amenities with support from the Pema Secretariat.
The clinic offers an increased access to evidence-based treatment and provide an effective referral pathway for persons with SUD through a continuum of care approach and strengthen peer-based recovery support services for people suffering from SUD.
Services: The following services are being provided;
- Intake and assessment of clients referred from RBP, OPD, ER and other health centers
- Individual, family and group therapy on selective days
- Peer support group meeting on Sundays
- Liaison and admission of clients for detoxification to psychiatric ward
- Facilitation and referral of clients with severe SUD problems for rehabilitation
- Clinical counseling to patients with mental illness

Staffing: The Medical Specialist is the head and clinical counselor as the In-Charge of this clinic. However, in absence of a clinical counselor, a psychiatric nurse working in medical ward takes charge of the unit providing services required. There are two peer counselors available during working hours to provide the regular services. Those staff who received hospital-based SUD treatment assist in taking therapy sessions whenever required.

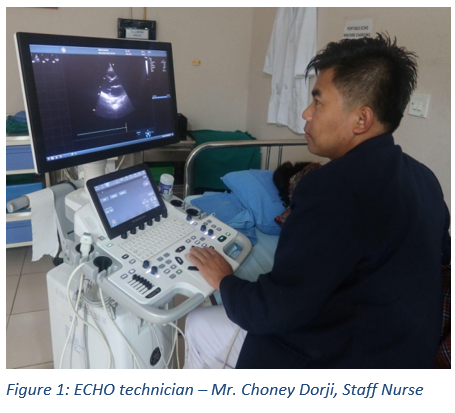
2. ECHO (Echocardiogram) Unit
Echo services was started on 13th March 2019 in ERRH and is manned by a lone cardiac sonographer till now. This diagnostic unit is located at chamber – 28. The services are available during working hours on weekdays while emergency services are provided 24X7 provided the sonographer is in station.
Services: The Following services are provided;
- Two dimensional echocardiography with color doppler imaging for OPD patients
- Portable two dimensional echocardiography with color doppler imaging for bedridden inpatients.
- ECG holter monitoring
3. TB/Leprosy Unit
The Tuberculosis Unit is located above the main hospital building, just below the vegetable shed. It was shifted to the current place in the year 2021 from the main hospital building.
Positive cases of Tuberculosis smear are admitted in the ward (drug susceptible) and MDR cases in MDR-TB ward which is located behind the main hospital building. It is a six bedded MDR-TB ward inaugurated in April 2023.

Services: The following services are provided:
- Preventive – Health talks to the public (once) monthly in the OPDs, as well as during the ORCs visit, which includes sign and symptoms, incubation periods, mode of transmission, duration of treatments, side effects of ATTs, follow up Schedules, contacts (family contact and close Contact), and identification of the DOTs provider after the discharge. Once a diagnoses of a TB case is made, an investigation is started involving a Doctor, Laboratory person, and TB focal person and reports are to be submitted to the TB program within 72 hours.
- Curative – Once the patient is diagnosed as smear positive, they are admitted and provide the DOTs as per the National TB guideline. ATTs are all issued from the TB unit. Health education is provided to the patient and DOTs providers before discharge.

Moreover, the unit also serves as the MDR-TB Registration Center for eastern districts. MDR-TB drugs are issued from center to the TB focal personal who have the MDR-TB cases as per the requisition.
The unit also function as Leprosy Unit for the surveillance, providing DOTS and also for follow up of all the old cases as per the protocol.
4. Non-Communicable Disease (NCD) Clinic
Non-communicable diseases (NCDs) is a result of a combination of genetic, physiological, environmental and behavioral factors and affects people of all age groups. Some common NCDs are hypertension, diabetes, cardiovascular diseases, cancers and chronic respiratory diseases.
About 74% of all deaths globally are attributed to NCDs and the prevalence is reported highest in low and middle-income countries. The NCD clinic of ERRH have around 2500 registered cases.
The leading metabolic risk factor is elevated blood pressure followed by raised blood glucose, and overweight and obesity. These diseases are driven by forces that include rapid urbanization, globalization of unhealthy lifestyles and population ageing. An important way to control NCDs is to focus on reducing the risk factors associated with these diseases. A comprehensive approach is needed requiring all sectors, including health, finance, transport, education, agriculture, planning and others, to collaborate to reduce the risks associated with NCDs, and to promote interventions to prevent and control them.
The Implementation of PEN HEARTS have immensely benefited the people in the rural communities in Mongar. Currently, Eastern Regional Referral Hospital serves as a NCD monitoring center for all 28 health centers within the district. The management of NCDs includes detecting, screening and treating these diseases, and providing access to palliative care for people in need.
